Best Practices for Disinfection in Healthcare Settings
Best Practices for Disinfection in Healthcare Settings

Keeping Germs at Bay: Best Practices for Disinfection in Healthcare Settings
In healthcare facilities, where the risk of infection is significantly heightened, maintaining rigorous disinfection practices isn't just a policy—it's a fundamental aspect of patient care. This blog explores the crucial strategies and protocols that medical facilities must adopt to ensure a safe environment for both patients and healthcare professionals.
Introduction: The Critical Importance of Stringent Disinfection
Healthcare-associated infections (HAIs) pose a significant threat in medical settings, affecting hundreds of thousands of patients annually. Effective disinfection practices are essential not only for preventing the spread of these infections but also for safeguarding the health of patients and staff alike. The goal is to create an environment where pathogens are continuously kept at bay.
Understanding Pathogens
Pathogens in healthcare environments can range from viruses and bacteria to fungi and protozoa. Common culprits include MRSA, E. coli, and influenza, which can survive on surfaces for hours to days, making disinfection a top priority. Understanding the nature and behavior of these pathogens is crucial for determining effective cleaning strategies.
Disinfection vs. Cleaning
While cleaning removes dirt and impurities from surfaces, disinfection goes a step further by using chemicals to kill germs. Sanitizing lowers the number of germs to a safe level as judged by public health standards or requirements. In medical settings, simply cleaning is not enough—disinfection is crucial to eliminate pathogens that cause disease.
Best Practices
Effective disinfection in healthcare settings involves several best practices:
Choosing the Right Disinfectants: Use EPA-approved disinfectants proven effective against a broad spectrum of pathogens.
Proper Use of Tools: Utilize disposable cleaning cloths and mops or those that can be disinfected to avoid cross-contamination.
Frequency of Cleaning: High-touch surfaces like doorknobs, bedrails, and medical equipment should be disinfected frequently, with schedules adjusted based on patient turnover and the area's infection risk.
Follow Manufacturer's Instructions: Ensure all disinfectants are used according to the manufacturer's directions, including contact times and dilutions, to maximize effectiveness.
Staff Training
Training staff in proper disinfection techniques is critical. This includes educating them on the correct use of disinfectants, understanding cross-contamination, and the importance of personal protective equipment (PPE). Regular training updates and assessments can help maintain high standards and adapt to new challenges.
Regulatory Compliance
Compliance with health standards and regulations is non-negotiable. Facilities should adhere to guidelines set by bodies like the CDC, WHO, and local health authorities. These regulations are designed to ensure that cleaning practices are thorough and meet the necessary standards to protect public health.
Conclusion
The importance of maintaining high standards of cleanliness and disinfection in healthcare settings cannot be overstated. It is directly linked to patient outcomes and the overall efficacy of the healthcare system. By adhering to best practices in disinfection, healthcare facilities can significantly reduce the incidence of HAIs, protect their staff, and provide safer care for all patients. The commitment to exceptional cleaning practices is a critical component of healthcare that requires diligence, proper resources, and ongoing education.
Chris Cassady
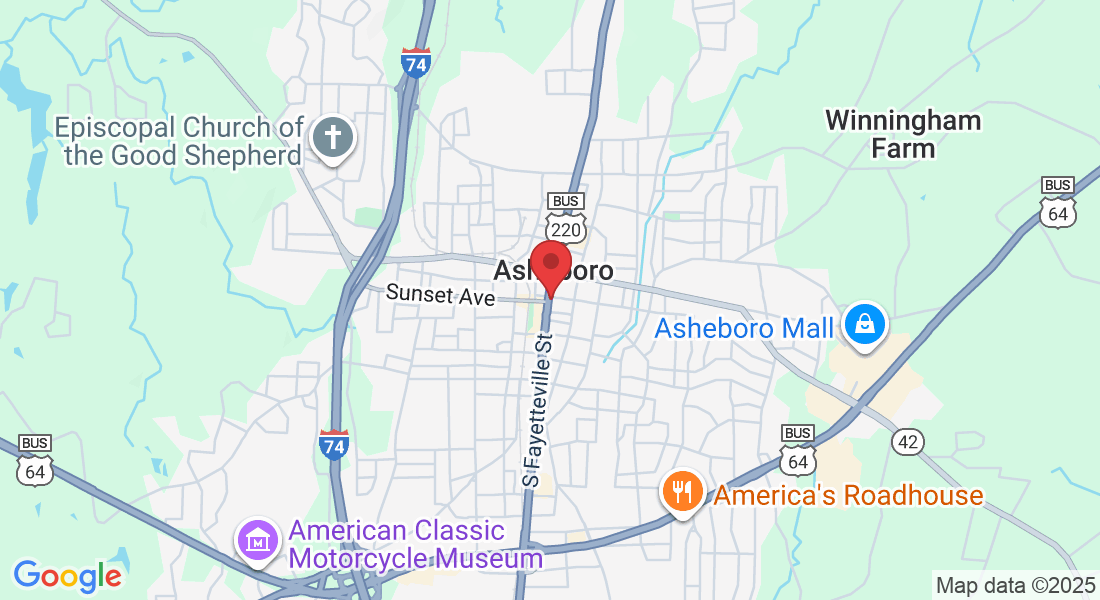
Empire Serv Inc
15 S. Fayetteville Street
Suite 203-F
Asheboro, NC 27203